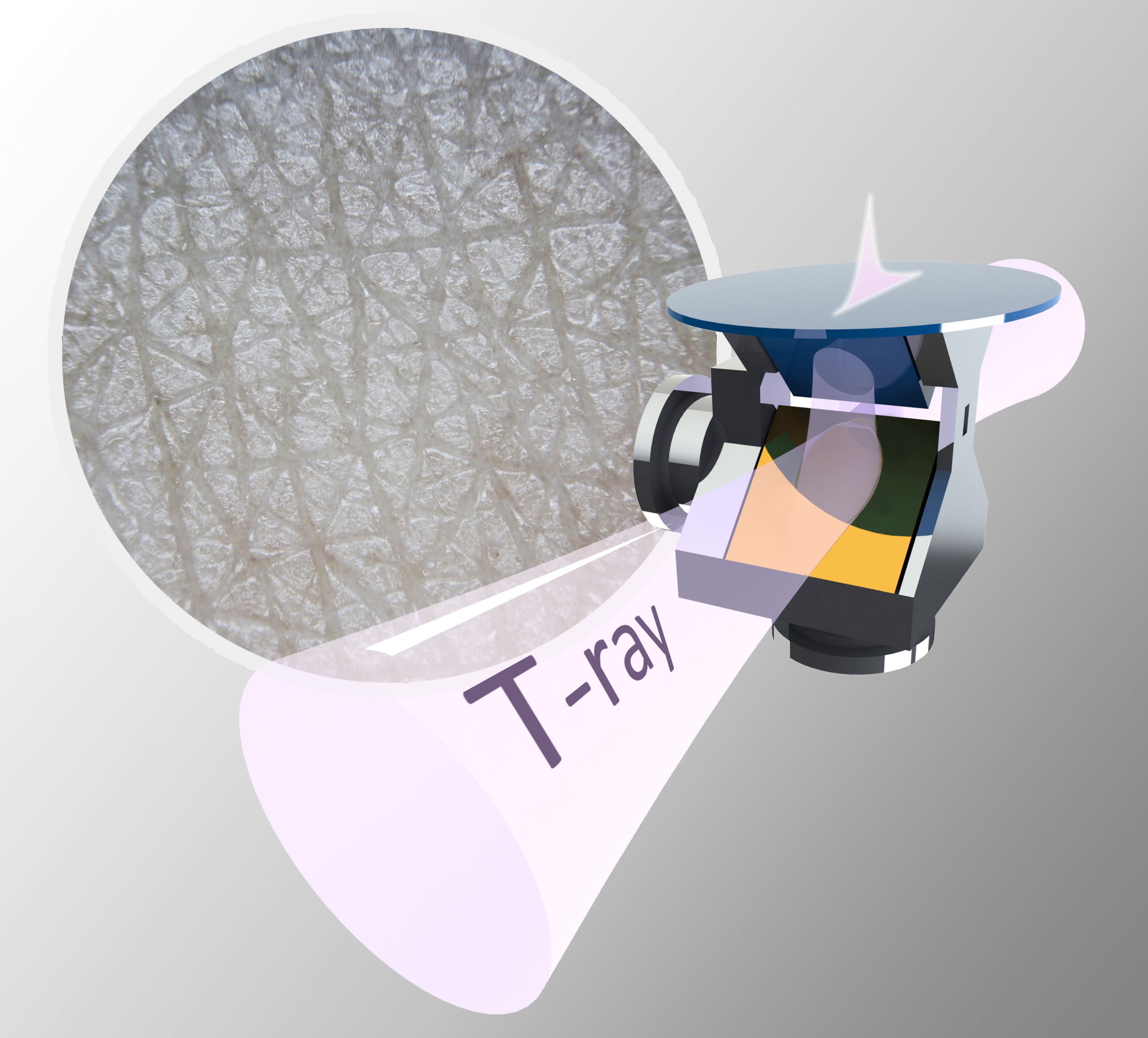
Scientists from the Faculty of Engineering at CUHK and the University of Warwick have developed a novel method for analysing the structure of skin using a type of radiation known as T-rays. It could build a more detailed picture of the structure of an area of skin and how hydrated it is than current methods allow, and help improve the diagnosis and treatment of skin conditions such as eczema, psoriasis and skin cancer. The finding has been reported in Advanced Photonics Research. Terahertz (THz) radiation, or T-rays, sit in between infrared and Wi-Fi on the electromagnetic spectrum. T-rays can see through many common materials such as plastics, ceramics and clothes, making them potentially useful in non-invasive inspections. The low energy photons of T-rays are also non-ionizing, making them very safe in biological settings including security and medical screening. Only the T-rays passing through the outer layers of skin (stratum corneum and epidermis) before being reflected back can be detected, as those travelling deeper are attenuated too much. Depending on the properties of the skin, those T-rays will be reflected back slightly differently. Scientists can then compare the properties of the light before and after it enters the skin. There are limitations in standard THz reflection spectroscopy, and to overcome these the scientists behind this new research used ellipsometry instead, which involves focusing T-rays at multiple angles on the same area of skin. In ordinary THz reflection imaging, the thickness and refractive index combine as one parameter. By taking measurements at multiple angles, the two can be separated. The team successfully demonstrated that using ellipsometry, they could accurately calculate the refractive index of skin, which determines how fast the ray travels through it, measured in two directions at a right angle. The difference between these refractive indices is termed birefringence – and this is the first time that the THz birefringence of human skin has been measured in vivo. These properties can provide valuable information on how much water is in the skin and enable the skin thickness to be calculated. Dr. Xuequan Chen, the study’s first author and post-doctoral fellow from the Department of Electronic Engineering at CUHK, said: “T-rays have been known to be sensitive to the hydration level of skin. However, we pointed out that the cellular structure of the stratum corneum also reacts to the THz reflections. Our technique enables this structure property to be sensitively probed, which provides comprehensive information about the skin and it is highly useful for skin diagnosis.” Professor Emma Pickwell-MacPherson, from the Department of Electronic Engineering at CUHK and the Department of Physics at the University of Warwick, said: “Hydrated skin will have a different refractive index from dehydrated skin. If you’re trying to improve skincare products for people with conditions like eczema or psoriasis, we will potentially be able to make quantitative assessments of how the skin is improving with different products, or differentiate types of skin. For skin cancer patients, you could also use THz imaging to probe the skin before surgery is started, to get a better idea of how far a tumour has spread, especially for those unseen as they are beneath the skin surface.” To test the novel method, the researchers had volunteers place their arm on the imaging window of their T-ray equipment for 30 minutes, after acclimatising to the ambient temperature and dryness of the laboratory. By holding their skin against the surface of the imaging window, they blocked water from escaping from their skin as perspiration, a process referred to as occlusion. The researchers then made four measurements at right angles to each other every two minutes over half an hour, so they could monitor the effect of occlusion over time. Because T-rays are particularly sensitive to water, they could see a noticeable difference as water accumulated in the skin, suggesting that the method could show how effective a product is at keeping skin hydrated, for example. Further research will look at improving the instrumentation of the process and how it might work as a practical device. Professor Pickwell-MacPherson said: “We do not have anything for clinical use that is accurate for measuring skin. Dermatologists need better quantitative tools to use, and use easily. If this works well, you could go into a clinic, put your arm on a scanner, your occlusion curve would be plotted and a suitable product for your skin could be recommended. We could get more tailored medicine and develop products for different skin responses. It could really fit in with the current focus on tailored medicine.” This work was funded by the Research Grants Council of Hong Kong, the Engineering and Physical Sciences Research Council (EPSRC), part of UK Research and Innovation, and the Royal Society. A full version of the paper can be found at: https://doi.org/10.1002/adpr.202000024 |
|